What we know is a huge proportion of our immune system resides in our GI tract.
Our introductory gut health course is about building the immune system against viral infection, disease and illness. This is one of those topics that is overwhelmingly MASSIVE and hard to even know where to start and that is why we started with an easy to understand course called ‘The Health of Your Gut”. You can check it out here where session one if free for you to decide to go ahead with the rest of the course.

Before going further and for your research, you could learn what the gut Microbiome is all about and how it plays a vital role in your immunity. Just like any other environment on the planet, our bodies have their own ecosystems — made up of 100 trillion microorganisms, or microbes, that live in and on our bodies. These include bacteria, fungi, viruses and other types of tiny organisms. It’s so large in fact, that the genes of microbes outnumber our body’s genes by 100 to 1.
Andrew Pekosz, a professor of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health has shared what the latest evidence shows and what researchers are working on to understand seasonality and immunity for COVID-19.
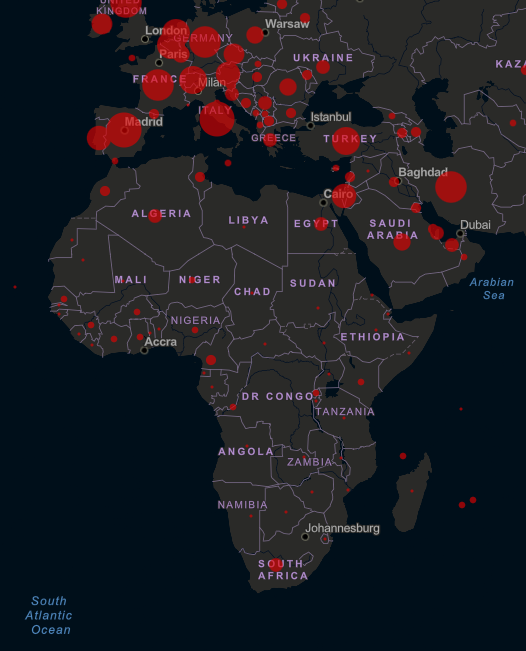
With the ongoing coronavirus pandemic that has infected over three quarters of a million people worldwide, with more than 1500 cases in South Africa and over 350,000 cases in the United States, laboratories around the world rush to develop treatments and vaccines for COVID-19.
Immunity against COVID-19
With COVID-19, and the current knowledge, there’s no one in the human population who has any level of immunity to the virus. So the percentage of people who are susceptible to COVID-19 is essentially 100%, whereas with influenza the percentage is significantly less than 100%. That’s one of the reasons why some of the stringent public health measures are being put into place.
Often, there are comparisons between COVID-19 and influenza because the symptoms are somewhat similar and because COVID-19 started to emerge in the winter, which is the same time of the year when we see influenza. But when it comes to immunity, there’s a very big difference between influenza and COVID-19. With influenza, because of previous infections and vaccinations, there’s always a percentage of the population that is immune to infection—so they’re protected and won’t get the flu that year. And there’s an even larger percentage of the population that has some immunity—not perfect immunity, so you’ll still get infected, but enough so that your symptoms will be relatively mild.
“THERE REALLY IS NOTHING ELSE THAT CAN PREVENT THIS VIRUS FROM SPREADING IN THE POPULATION OUTSIDE OF PUBLIC HEALTH INTERVENTIONS LIKE SOCIAL DISTANCING. IT’S THE LACK OF IMMUNITY IN THE POPULATION THAT IS MAKING PEOPLE SO SUSCEPTIBLE.” Andrew Pekosz Professor of molecular microbiology and immunology
Why is it that older people are developing more severe symptoms than younger people, even though both groups have no immunity to COVID-19?
There is no good answer for that yet. It certainly seems that people over the age of 60, particularly those with secondary medical conditions, are at greater risk for severe disease. We’re beginning to understand that men may also be at increased risk. We’re seeing these trends pretty consistently across different countries.
According to Tirumalai Kamala, a Ph.D. in Microbiology from India, for the following reasons, the immune system’s ability to be effective in its responses and to be judicious in its choice of targets wanes with age.
- Aging goes hand in glove with potentially irreversible maladaptive alterations in metabolism. The resultant cascade effect on nutritional status in turn profoundly affects immune function directly as well as indirectly through its effect on microbiota.
- The body’s immune history, a lifetime of fighting off infections, comes with a price – the memory compartment of the adaptive immune system expands at the expense of its naive counterpart – less prepared to fight off newer, unanticipated threats.
- The price the aging immune system pays for its history is compounded by the steep toll persistent viruses – the immune system can deal with such persisters handily at younger ages when its regenerative capacity is in full bloom. However, such capacity shrinks dramatically with age.
- As a consequence of creeping ‘immunodeficiency’, such aging-related changes tax the immune system’s ability to be effective and to choose its targets judiciously, making itLess capable of fighting off new infections.
- Less stringent in its immunosurveillance against the antigenic products of mutant cells that could be potentially malignant. Such failure could stoke cancer.
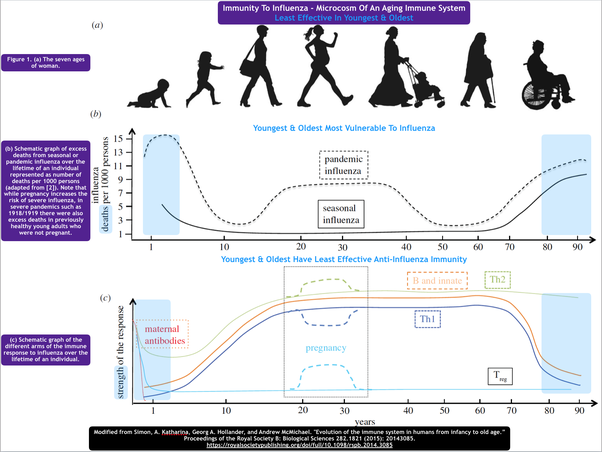
The immune system is less capable of maintaining full tolerance to its own body, which could result in autoimmunity.
What’s the role of seasonality in the spread of this virus?
At the present moment it is not known if COVID-19 will be very dependent on winter to effectively transmit, like the flu, or if it will find ways to effectively transmit throughout the year. If we look to the Southern hemisphere, we’re seeing significant COVID-19 outbreaks even though this is their summer season. So it’s expected that the virus is going to be able to transmit here at least to some extent after the winter months.
There is a major concern about what will happen if public health interventions are loosened. Right now, public health interventions are doing a good job of reducing the number of cases, but it is not known don’t know how long we will have to keep those measures in place. When we relieve them, there is always a potential for cases to spike again.
Other aspects of COVID-19 are researchers trying to understand
Researchers are trying to understand how this virus is able to cause many more cases of mild disease compared to other viruses. The thinking is that it may be linked to why it’s so good at transmitting. They also trying to understand, once you’ve had the virus, whether you’re safe to go out and work again because you have some level of protection.
Researchers are seeking ways to understand what the true infectious time is and how to shorten the time that someone has to be in quarantine, that would help with workforce issues. Our take on this is build your immunity to optimal and allow the body to respond to the viral infection.
With what we are being presented with COVID-19, many are fearful as they are not certain about how their immune system will respond. You can build your immune system one step at a time. the first best thing you can do is not so much what to add but rather what you can remove that is putting your immune system under greater strain.
We will shortly release the best of the best suggestions to enhance your immune response a a viral infection, illness and disease.
Bibliography
1. Boraschi, Diana, et al. “The gracefully aging immune system.” Science translational medicine 5.185 (2013): 185ps8-185ps8. https://pdfs.semanticscholar.org…
2. Franceschi, Claudio, et al. “Inflammaging: a new immune–metabolic viewpoint for age-related diseases.” Nature Reviews Endocrinology (2018): 1. http://www.mr-gut.cn/s/pf/180727…
3. Lee, Naeun, Min Sun Shin, and Insoo Kang. “T-cell biology in aging, with a focus on lung disease.” Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences 67.3 (2012): 254-263. T-Cell Biology in Aging, With a Focus on Lung Disease